Tom Neltner, Senior Director, Safer Chemicals
This is the fourth in our Unleaded Juice blog series exploring how the Food and Drug Administration (FDA) sets limits for toxic elements like lead, arsenic, and cadmium in food and the implications for the agency’s Closer To Zero program.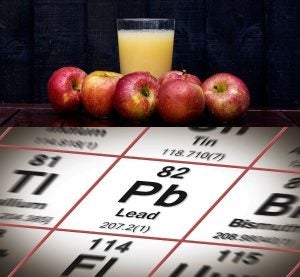
In June, after issuing its proposed action levels for lead in juice, FDA tightened its Interim Reference Levels (IRLs) for lead to 2.2 µg/day for children and 8.8 µg/day for females of childbearing age—a drop of 27% from the original IRLs it established in 2018. We estimate this change increased the number of children over the IRL for lead from 1.2 million to more than 7 million.
The agency describes IRLs as daily maximum intake levels for lead in food and beverages. FDA scientists said the change was made to match the Centers for Disease Control and Prevention’s (CDC) October 2021 revised blood lead reference value. This value is commonly known as the elevated blood lead level (EBLL).[1] FDA uses the “interim” label in recognition that there is no known safe level of exposure to lead and the neurotoxic harm it can cause. FDA anticipates matching the IRLs to future reductions in CDC’s reference value as the U.S. makes progress in reducing children’s exposure to lead.
We applaud FDA’s decision to tighten the IRLs. It is a good example of the type of continuous improvement to which FDA committed in its Closer to Zero Action Plan, which aims to lower levels of lead, cadmium, mercury, and inorganic arsenic in food that babies and young children eat and drink.
The challenge now is to translate the tighter daily maximum intake level into action levels for specific foods. Next steps for FDA should include:
- Further tightening its recently proposed action level for lead in juice.
- Using the revised lead IRLs as:
- The basis for its proposal for foods commonly consumed by babies and young children – currently stuck in the review process at the White House’s Office of Management and Budget (OMB).
- A model for FDA’s anticipated IRLs for inorganic arsenic and cadmium under its Closer to Zero program.









