Note: This blog has been updated and adapted. For the most up-to-date information, please visit our new page, Top 10 Cities with the Most Lead Pipes.
Roya Alkafaji, Manager, Healthy Communities and Tom Neltner, Senior Director, Safer Chemicals Initiative
EDF identified 10 cities in the U.S. with the most lead service lines (LSLs) based on numbers reported in 2021.[1] These cities collectively have over one million LSLs, representing 12% of the 9.2 million EPA estimates are in the country.
Below we rank each city from most LSLs to fewest, and briefly describe the progress each city has made toward LSL replacement. Some have robust programs, while others have yet to start addressing the problem.
The List
1. Chicago, IL
Chicago Department of Water Management reported 387,095 LSLs in 2021, more than twice as many as the next city on this list. Three-quarters of its service lines are LSLs, and virtually all the rest are of unknown material. City ordinance actually mandated that LSLs be installed until the federal government banned them in 1986.
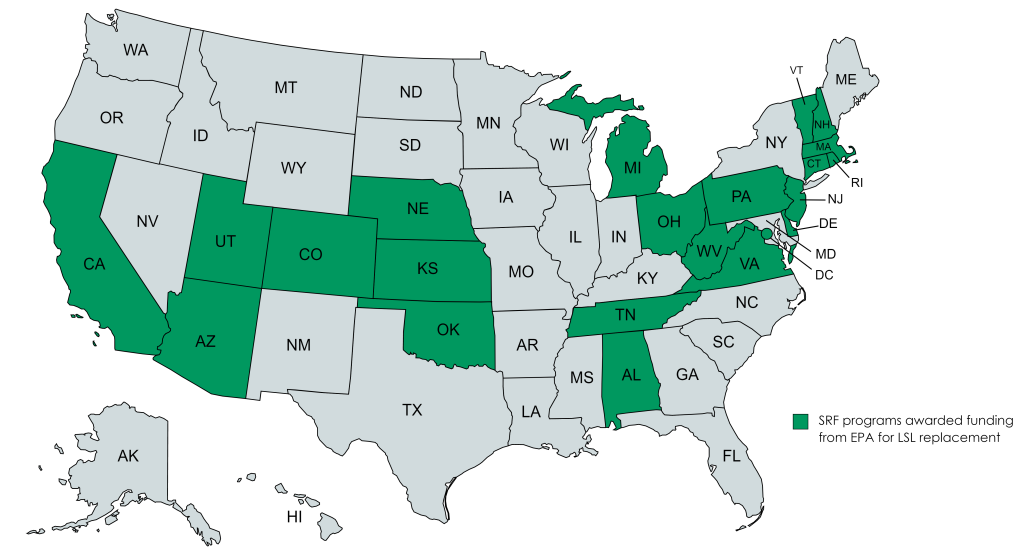
Decades later, Chicago is struggling to pull itself out of a deep hole relative to most other large cities that took earlier action against lead pipes. Chicago has a small LSL replacement program but applied for a $336 million loan from EPA in 2020[2] and $8 million in state revolving funds (SRF) from Illinois EPA in 2023 to accelerate the effort.
2. Cleveland, OH
Cleveland Water reported 185,409 LSLs in 2021, about 43% of all its service lines.
The utility has a small LSL replacement program but is seeking more than $63 million in federal infrastructure funding from Ohio EPA in 2023 to accelerate the effort.
3. New York, NY
New York City reported 137,542 LSLs in 2021 and an additional 230,870 lines that are of unknown material. About 43% of the city’s service lines are lead or of unknown material.
It has a small LSL replacement program and is seeking more than $58 million in federal infrastructure funding from New York State DEP in 2023 to accelerate the effort.